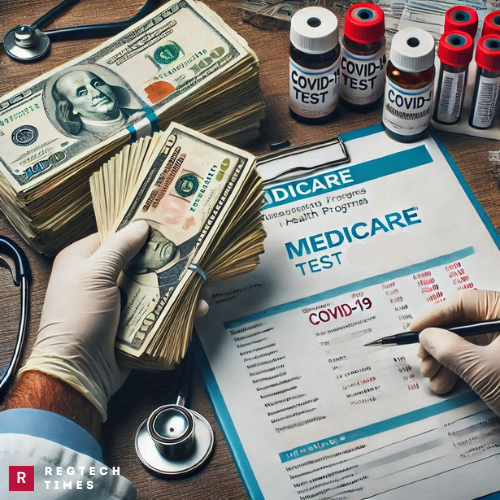
In a shocking case of health care fraud, Dr. Mark Mazzare, a 57-year-old physician from Tyler, Texas, pleaded guilty for his role in a $5.5 million scheme involving over-the-counter (OTC) COVID-19 test kits. The scheme, which ran from late 2022 to mid-2023, resulted in millions of dollars in false claims submitted to Medicare.
According to court documents, Dr. Mazzare illegally purchased private Medicare beneficiary information to carry out his plan. This sensitive data, referred to as Beneficiary Identification Numbers (BINs), was bought under the disguise of so-called “lead packages” from a fake marketing agreement. The goal was to hide the true nature of the transaction.
Once he obtained the BINs, Dr. Mazzare worked with others to fraudulently bill Medicare for COVID-19 test kits. Many of these test kits were never requested or even needed by the individuals whose identities were used. To make the scheme look real, the fraudsters created fake audio recordings that were designed to sound like Medicare beneficiaries asking for the test kits. These recordings, however, were completely fabricated.
Jose Goyos and Co-Conspirators Behind Massive $67M Health Care Fraud
Between November 2022 and June 2023, Dr. Mazzare used the illegally purchased Medicare details to submit over $5.5 million in claims for these COVID-19 test kits. Out of that amount, Medicare ended up paying approximately $3.44 million before the fraud was discovered.
Details of the Fraud: How the Scheme Worked
The scheme was simple yet harmful. Dr. Mazzare, who should have been helping patients, instead misused private medical details for his personal gain. He obtained private Medicare information illegally and used it to make fake requests for COVID-19 tests. These requests made it appear as if real Medicare beneficiaries were asking for the tests, but in reality, many had no idea their information was being misused.
To cover his tracks, Dr. Mazzare entered into a fake agreement with a so-called “marketer.” On paper, it looked like he was purchasing legitimate marketing leads. However, these “leads” were just stolen Medicare IDs. As part of the scam, fake audio recordings were also created to give the illusion that the beneficiaries were ordering the COVID-19 test kits themselves.
Once Medicare received these fake orders, the government health program paid out claims, believing the test kits were medically necessary. However, most of the kits were completely unnecessary. In many cases, the people who supposedly “requested” the kits never even received them or had no use for them.
Dr. Mazzare’s actions not only cost taxpayers millions of dollars but also put the trust in government health programs at risk. The fraud highlights how critical private medical information can be misused when it falls into the wrong hands.
Reis and Hockridge Charged in Massive COVID-19 Relief Fraud Scheme
Legal Action: What Happens Next?
Dr. Mark Mazzare pleaded guilty to two serious charges: conspiracy to defraud the United States and the illegal purchase, sale, and use of Medicare beneficiary information. For these crimes, he faces a maximum penalty of five years in prison. The exact sentence will be determined later by a federal district court judge, who will consider sentencing guidelines and other legal factors.
The case was announced by top officials from the Justice Department’s Criminal Division, the U.S. Attorney’s Office for the Eastern District of Texas, the Department of Health and Human Services Office of Inspector General (HHS-OIG), and the U.S. Postal Inspection Service (USPIS). These agencies played a major role in uncovering the fraud and bringing Dr. Mazzare to justice.
The investigation was carried out by HHS-OIG and USPIS, with additional assistance from the Texas Attorney General’s Medicaid Fraud Control Unit. Prosecutors from the Justice Department’s Fraud Section and the Eastern District of Texas are handling the case in court.
This case is part of a larger effort by the Health Care Fraud Strike Force Program, which was launched in 2007 to fight fraud against federal health care programs. Over the years, this program has charged more than 5,400 people who have collectively stolen over $27 billion from federal health care systems. Agencies like the Centers for Medicare & Medicaid Services are also working to hold providers accountable and prevent future fraud.